Audience members on Tuesday morning helped advance a step-by-step exploration of intermediate-risk pulmonary embolism that blended a fictional case study with quiz questions and expert panel discussion.

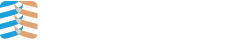
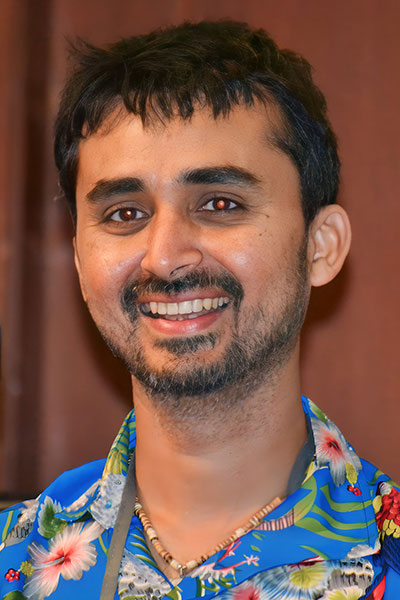
The session, An Innovative, Highly Interactive Discussion of Intermediate-Risk Pulmonary Embolism, was co-chaired by Lisa Moores, MD, FCCP, Associate Dean for Student Affairs at the Uniformed Services University of the Health Sciences School of Medicine in Bethesda, Maryland, and Parth Rali, MD, MBBS, Associate Professor at the Lewis Katz School of Medicine at Temple University.
They were joined on the panel by Shari Brosnahan, MD, Assistant Professor at NYU Grossman School of Medicine; Bushra Mina, MD, FCCP, Chief of the Pulmonary Medicine Division at Lenox Hill Hospital, New York City; and Janine Vintch, MD, FCCP, Professor of Clinical Medicine at the David Geffen School of Medicine at UCLA.
Dr. Moores presented a case study of a 38-year-old previously healthy male who fell while riding his bike and hit his head. He briefly lost consciousness, and his head CT was normal. Additional vital statistics included:
- Requiring 5 LPM for SpO2 96%
- HR 122
- SBP 100/64
She then directed audience members to answer multiple-choice questions via QR code.
Based upon this information, how would you initially categorize this patient?
Most audience members said they needed more information about the patient before identifying his risk.
“I think it’s reasonable based on some of the information that I gave you that you would put this patient in an intermediate category,” Dr. Moores said. “Whether they’re low or high risk, I’m not sure we have enough information to say at this point.”
Dr. Moores asked the audience the next question.
If you incorporated imaging to help you in your assessment, which of the following applies?
Choices included interpreting a CT pulmonary angiogram; performing point-of-care ultrasound; ordering an echocardiogram; any of the above; or using only risk scores and not imaging. No single option stood out after the audience vote.
Dr. Mina weighed in, saying the CT scan can offer information about the burden of the clot, the distribution, and whether it is lobar or segmental.
“It gives you information for risk stratification, it can give you an idea about the mortality, and also it can give you an idea if we’re dealing with acute on top of chronic,” he said.
Dr. Rali opted for point-of-care ultrasound and echocardiogram, saying they answer some of those questions as well. And a CT scan has limitations.
“A CT does not pick up the clot in transit,” he said.
Dr. Moores offered more information on the case study:
- Positive troponin
- LA 2.3
- sPESI score 3
- CTPA RV/LV 1.1
- Echo: Moderately dilated RV
Based on the new information, she asked another question of the audience:
What therapy would you initiate at this time?
Audience members were given the option of low molecular weight heparin (LMWH), heparin with or without bolus, direct oral anticoagulants, and inferior vena cava (IVC) filter. Close to 60% of respondents chose LMWH, with the rest choosing heparin with a bolus.

Dr. Brosnahan supported using heparin with a bolus despite the majority vote for LMWH.
“On the outside of the clot, there’s actually antithrombin, and you can have mild heparin resistance or major heparin resistance depending on the patient, and you aren’t as aware of that with low molecular weight heparin,” she said.
An audience member pointed out that patient’s blood pressure is an issue, and Dr. Moores agreed.
“I think your point about blood pressure is an excellent one, particularly since we don’t know the baseline blood pressure of this patient,” she said.
Dr. Moores added one more relevant vital statistic to the case study: the patient has a bilateral proximal deep vein thrombosis and acute kidney injury.
What would you do for this patient?
The choices were:
- Anticoagulation only
- Anticoagulation with IVC filter
- Catheter-based treatment
- Half-dose tissue plasminogen activator (tPA)
- Full-dose tPA
- ECMO
- Surgical embolectomy

Forty percent of the respondents voted for a catheter-based treatment, while most of the other respondents chose anticoagulation or anticoagulation with IVC filter.
Dr. Vintch said she would go with anticoagulation at this point.
“While he has some features that are concerning, I think he’s young and I still have some time to observe him,” she said. “I am going to make sure the radiologist and cardiologist are available and aware, though.”
Dr. Moores wrapped up the session by recognizing that there is still a lot to learn.
“It’s actually why I’m in this field,” she said. “There’s still a lot we don’t know that does involve our clinical judgment.”