Asthma and COPD share many attributes. However, professional opinions diverge on whether there is a middle ground or overlap in these two conditions, as there is no universally accepted definition of the overlap. Treatment strategies for patients who present with traits of both diseases are also controversial.

Four experts in asthma and COPD took positions on two topics during the Sunday morning session, Controversies in Asthma-COPD Overlap: A Pro-Con Debate: whether asthma-COPD overlap (ACO) exists and whether health care professionals should take a “treatable traits” approach to managing patients’ diseases. Neveda Murugesan, MD, Pulmonary and Critical Care Fellow at the Baylor College of Medicine, moderated the session.
Asthma-COPD overlap—or distinct diseases?

Nicola A. Hanania, MD, MS, FCCP, Professor of Medicine and Director, Airways Clinical Research Center, Baylor College of Medicine, began the discussion by taking the “pro” position that asthma-COPD overlap exists. He cited the “Dutch hypothesis,” which considered asthma and COPD as a spectrum of one disease, and an opposing hypothesis from a British researcher that stated the opposite: They are two different diseases with different risk factors.
He garnered laughs by showing that Wikipedia and ChatGPT agree with him that overlap exists before explaining more seriously that the overlap has been scientifically recognized for the past 10 years.
“It is often challenging to diagnose, but it’s important as a pulmonologist to understand and agree that this entity does exist,” Dr. Hanania said. “It has a clinical implication and treatment implication, and there may be some shared physiologic and pathologic features between asthma, COPD, and asthma-COPD overlap.”
He said it is important that it receive more attention in the lab.
“We need larger longitudinal studies to understand the natural history of patients with ACO,” Dr. Hanania concluded.
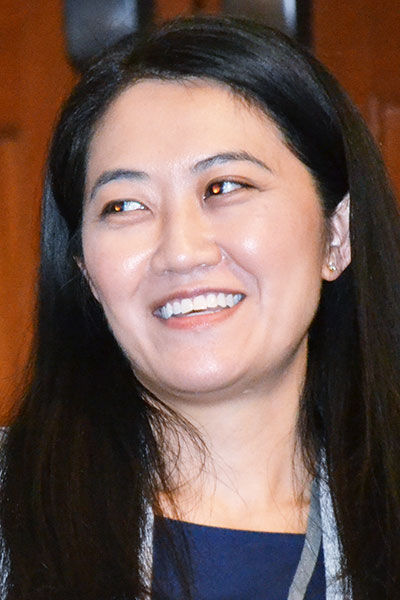
Garbo Mak, MD, Clinical Assistant Professor, Division of Pulmonary, Critical Care and Sleep Medicine, University of Washington, took the “con” position of the controversy, pointing out that each disease has distinct features, and that diagnosing overlap has shortcomings in clinical application and use.
“It is very important to recognize separate entities and separate diagnoses,” Dr. Mak said. “The reason for this is because having a diagnosis helps guide treatment and sets expectations about prognosis, and it also facilitates communication among clinicians.”
One of the issues with the existence of the asthma-COPD overlap is that it isn’t clearly defined—patients often receive one diagnosis but have various features of the other.
“This really highlights how diverse a patient population this can include, and how nonspecific, and it probably lacks a lot of clarity,” she said.
Dr. Mak concluded that asthma and COPD are distinct and separate, although they may co-exist in an individual, and they may share some features.
“We should call a condition what it is,” she said. “And we should be using the guidelines we have in place for both of these conditions.”
Applying the treatable traits approach in asthma and COPD
The concept of treatable traits in asthma, COPD, and an overlap of the two also remains controversial as professionals debate what is most effective for patient outcomes.

Peter G. Gibson, MBBS, DMed, Conjoint Professor of Medicine at the University of Newcastle, Australia, took the “pro” position and provided some evidence supporting treatable traits as a strategy.
Clinicians start by learning diagnosis, but once they start in practice, they must go beyond diagnosis, he said.
“When you move away from the disease to managing the patient in front of you, increasingly that management is about what are the individual problems in this person that I can address that will improve this person’s health,” Dr. Gibson said.
He provided ways to manage a treatable traits model of care in individual practices, and he outlined operational tools, including using case managers, multidisciplinary teams, and structural assessments. Ultimately, it results in better quality of life for patients, he said.
“It’s more effective than step care, and it is the standard of care for severe asthma and COPD,” he said.
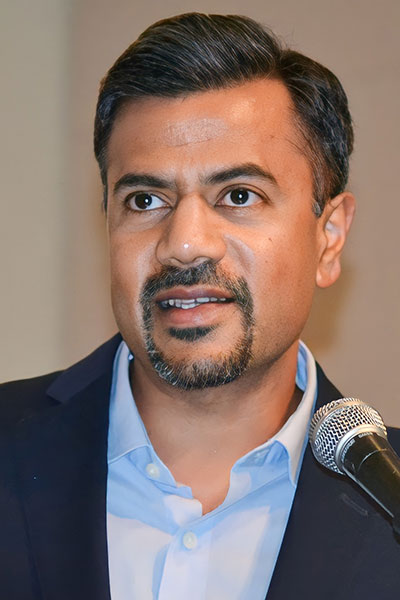
Arjun Mohan, MD, Associate Professor of Medicine, University of Michigan, took the “con” position and argued that the treatable traits approach is not a strategy. He noted that many of the traits that are part of the discussion are non-pulmonary, and instead are behavioral. He encouraged reassessment before moving forward further with the strategy.
“We miss a lot if we focus on single traits rather than treating the whole disease,” he said. “The evidence does not support large-scale uptake of it.”
Dr. Mohan stated that while the treatable traits approach is a novel concept, it is not ready for a larger role in treating asthma and COPD.
“I hope that future randomized controlled trials pretty much blow my slide deck out of the water, but I don’t think we’re there yet,” he said.
Join us at CHEST 2025
Save the date for the next Annual Meeting, October 19 to 22, 2025, in Chicago. CHEST 2025 will explore the latest advancements in pulmonary, critical care, and sleep medicine, with a focus on innovation and the future, just as the city itself embodies progress and reinvention.





