The COVID-19 pandemic upended the practices and lives of CHEST members—and changed CHEST 2020 into a virtual meeting—so it’s fitting that this year’s Opening Session focused on the defining global event of the year.
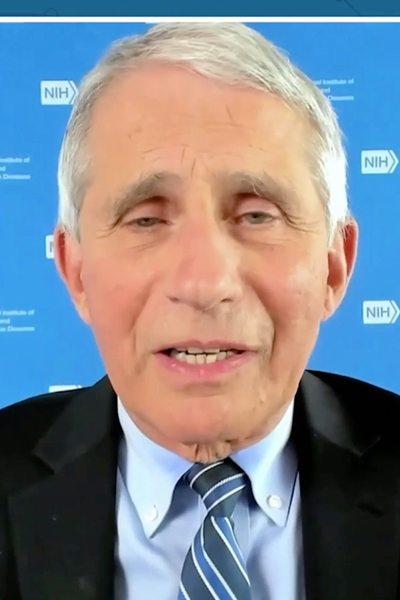
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases at the US National Institutes of Health, delivered this year’s keynote address on Sunday, October 18. The session will soon be available for on-demand viewing on the virtual CHEST 2020 meeting platform through January 18, 2021, for registered attendees.
Dr. Fauci delivered an overview of the public health and scientific challenges of the SARS-CoV-2 virus and the COVID-19 disease it causes. Before diving into those topics, however, he offered a special tribute to all of the CHEST members who have worked tirelessly during the pandemic and remained dedicated to patient care.
“At great risk to your own health, your teams have been at the forefront of the COVID-19 response, offering expert care and compassion to patients who not only are sick but also separated from their loved ones,” Dr. Fauci said. “Additionally, as a medical society, your members have collaborated to produce valuable resources that health-care professionals everywhere can use to increase their clinical knowledge base and raise their level of care. CHEST has demonstrated how to be a global leader during a historic public health emergency.”

The NIH has created a treatment guidelines panel that brings a group of COVID-19 clinical care experts together, Dr. Fauci said, to work on a “living document.” The panel meets frequently to update the document, which covers the latest clinical data and current recommendations for treating and caring for COVID-19 patients. Those recommendations can be found at Covid19treatmentguidelines.nih.gov.
Dr. Fauci reviewed treatments that the panel now recommends—the antiviral remdesivir and the corticosteroid dexamethasone—and other treatments still under investigation. One of those treatments under investigation, monoclonal antibodies, has provided some exciting data, he said. Inpatient and outpatient clinical trials continue, and there’s evidence that may show monoclonal antibodies could offer family prophylaxis if a family member is infected with COVID-19, or even as a broad primary prophylaxis in the nursing home setting.
In the search for a vaccine, five candidates are already in phase III trials thanks to an unprecedented national approach to harmonizing protocols to commend data and safety monitoring, common primary and secondary endpoints, and common immunologic parameters. Dr Fauci said he remains “cautiously optimistic” that there will be a safe and effective vaccine ready by the end of the year.
“Given the rate of infection that’s going on in this country and the distribution of the clinical trial sites involving tens of thousands of volunteers, we project that we will have an answer as to whether or not we have a safe and effective vaccine by November or December,” he said.
Dr. Fauci also noted a clear and disturbing ethic disparity not only in the incidence of COVID-19 infection but also in the seriousness of complications and hospitalizations for African Americans, Latinx, Native Americans, Alaskan native populations, and Pacific Islanders when compared with white populations.
CHEST leaders follow Dr. Fauci’s talk with Q&A
Following Dr. Fauci’s talk, a panel featuring CHEST President-elect Steven Simpson, MD, FCCP, Chair of the CHEST COVID-19 Task Force; Mangala Narasimhan, DO, FCCP, director of critical care services at Northwell Health; and Cmdr. Ryan Maves, MD, FCCP, critical care specialist at Naval Medical Center San Diego, took part in a COVID-19 question-and-answer session.
Dr. Narasimhan said that lessons learned during the start of the pandemic will help ease the severity of surges such as the one currently happening in many places around the US. During the peak in March and April, Northwell saw more than 900 patients intubated, and that’s now closer to 30 patients. There was also trouble determining which caregivers would care for COVID-19 patients and struggles with supply chains. There was more guessing about treatment and a greater sense of fear overall.
“The first time around, everybody was petrified that we were bringing this home to our families and to ourselves,” Dr. Narasimhan said. “We now know that some treatments work, and we have some good clinical trials. We know that noninvasive [treatment] is a real option, which we didn’t know the first time around. So we have more tools in our toolbox. We have some good treatments, and we have the luxury of not as many patients, which really was our big issue the first time around.”
CHEST President Stephanie Levine, MD, FCCP, moderated the question-and-answer session and also helped start the session with an overview of her year as president.
From the beginning of her term as president, CHEST members have had to reimagine what daily practice looks like. At the start of her term, Dr. Levine said that she wanted CHEST to be the welcoming home for interprofessional health-care team members wanting the best educational experiences that lead to the best patient outcomes, and the pandemic made it even more imperative to come together for advice, guidance, resources, understanding, empathy, and a sense of community. CHEST members have met that challenge.
“You are innovative problem solvers who inspire me and show me how much purpose there is in what we do,” Dr. Levine said. “You know that, ultimately, it’s about providing outstanding clinical care and compassion to our patients, and you’ve proven that, especially during this time when our stress levels are high, the hours are long and our personal needs have been sacrificed.”





