Hosted by CHEST President-Elect David Schulman, MD, MPH, FCCP, the final round of this year’s Pardon the Interruption: Controversies in Critical Care competition pitted semifinal round winners Ronald Goldenberg, MD, of NYU Grossman School of Medicine, and Gabriel Bosslet, MD, FCCP, of Indiana University School of Medicine, against the reigning 2020 champion Kristin Burkart, MD, MS, FCCP, of Columbia University School of Medicine.
Now in its fourth year at the annual meeting, Pardon the Interruption challenges three colleague-competitors to a rapid-fire Q&A about clinical situation in critical care. Each speaker has a minute to present their expert opinions and any supporting data as Dr. Schulman scores their answers. Topical knowledge, rhetorical flair, and “sass” all factor into the scoring.
Questions ranged from broad approach-based strategies to specific treatment decisions. Answers from the competitors and the ensuing arguments ranged from subtle differences on nuances or details to adamant, and sometimes aggressive, disagreements. Many of the arguments came down to support of evidence based on clinical trials vs observations and opinions based on real-world clinical experience.
For example, with the first question—”What is the role for empiric anticoagulation in critically ill COVID patients, and at what degree of anticoagulation?”—Drs. Bosslet and Burkart both cited recent studies and argued that the risk of bleeding outweighs any potential benefits of therapeutic anticoagulation in these patients. Dr. Goldenberg, on the other hand, took the lone stance that, once these patients reach the ICU, the risk of clots outweighs the risk of bleeding.
“At this point in time, prophylactic anticoagulation should be given in critically ill patients, but not therapeutic anticoagulation—there have been a couple studies that have demonstrated this,” Dr. Bosslet said. “What’s weird is that it looks like therapeutic dose anticoagulation for those who are low risk may actually have some benefit in people before they get to the ICU, but once they get to the ICU and the cat’s out of the bag with the inflammatory cascade, it doesn’t look like it does much. So we, as intensivists should not be starting therapeutic dose anticoagulation just for COVID.”
“As far as I’m concerned, I don’t think they bleed, but they do clot. Studies have shown no downside and maybe some upside in mild to moderate patients before they get to the ICU, and to me, nothing changes when they do get to the ICU except, if anything, they’re sicker,” Dr. Goldenberg said. “At least half our patients will have DVTs and then we’re forced to anticoagulate them. If you’re really worried about the bleeding, use some low-dose heparin. I know from my ECMO patients who are on anticoagulation, we haven’t seen any increased risk of bleeding and they’re all anticoagulated, so I’m not worried about a little bit of heparin.”
“I’m going to have to side with Gabe on this one,” Dr. Burkart said. “For critically ill patients, there is an increased risk, although not statistically significant, for bleeding. Anecdotally, we’ve seen them both bleed and clot in our unit, so I think we have to be very careful and we have to look at our large trial data for support.
The data says that in the ICU, they’re past the cascade and the inflammation and that increased risk of bleeding outweighs the benefits. They should be treated if you diagnose a clot and/or have a high suspicion of clot, but not just all comers with COVID should be put on therapeutic anticoagulation.”
A subsequent question—”Is targeted temperature management for out-of-hospital cardiac arrest dead, or not?”—turned the tables a bit and found Dr. Bosslet in strong disagreement with both Drs. Burkart and Goldenberg.
Dr. Bosslet cited recent results from the European Targeted Temperature Management after Cardiac Arrest 2 (TTM2) trial, which looked at targeted hypothermia vs targeted normothermia after out-of-hospital cardiac arrest, to support his argument that targeted temperature management, at least at the 33°C level, is indeed dead, while Drs. Burkart and Goldenberg contended that it is alive and well and should remain so.
“I don’t think it’s dead at all and, in fact, I think the biggest thing that’s changed for neurologic outcome is targeted temperature management,” Dr. Goldenberg said. “We have to remember why we do it. We do it to decrease oxygen and ATP demand in the brain and decrease cerebral metabolism and prevent cerebral edema, and for every degree you lower the temperature, you get a decrease of cerebral metabolism by 6%. The single best thing for preserving neurologic outcome is making them cold, and I think everyone should be at 33 degrees.”
“I don’t care what number you pick or choose— it’s all targeted temperature management, so even if people want to stand in a line behind that 2021 paper that came out for normothermic, 50% of those patients required active cooling to keep them at normothermic,” Dr. Burkart said. “In 2020, several studies looking at outcomes now since we switched from 33 to 36 degrees, showed that there has been worse survival and worse neurologic outcomes.
“I cannot believe that both of you guys came down against TTM2— this was a really flawlessly executed study,” Dr. Bosslet said. “I think you can argue that 36 degrees might still be alive, but I don’t consider that temperature management, that’s just aggressive avoidance of fever. To me, you’re ignoring data. I’m flabbergasted that you guys came down on the side of targeted temperature management.” (Note: Dr. Bosslet was awarded 1 point by Dr. Schulman for using the word “flabbergasted.”)
Following are the other questions the competitors addressed:
- What is the appropriate timing for initiation of renal replacement therapy in acute kidney injury?
- Does full isolation for mechanically ventilated COVID patients detract from outcomes and, if so, what should we do about it?
- What is the role of midodrine in the management of shock?
- Is there a need to better manage the circadian rhythm in the intensive care unit, and does it impact outcome?
- Should lung transplant be “on the table” for patients with refractory COVID?
- Should a bougie be used for most or all first-pass intubation attempts?
- What is the correct steroid dose for COVID-related respiratory failure? 6mg? 20mg?
Following the final question, Dr. Schulman invited fellow judge Alex Niven, MD, FCCP, to join the discussion for a “debrief” of the most controversial topics covered during the competition and invited the audience to post in the chat box who they thought won.
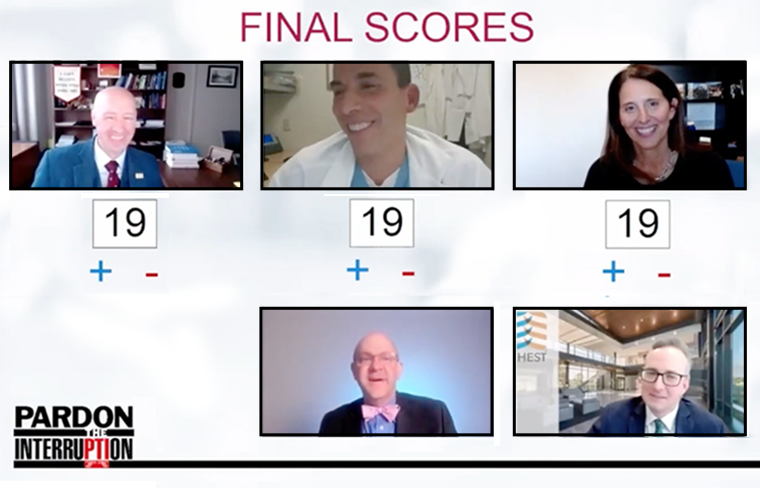
After careful deliberation and a tally of the audience picks, Dr. Schulman announced that Dr. Burkart edged out her opponents and retained the Pardon the Interruption championship for another year. She will have the opportunity to make it three in a row when she defends her title next year at CHEST 2022 in Nashville.
ACCESS SESSIONS ON DEMAND
Registered CHEST 2021 attendees have continued access to 200+ educational sessions until October 1, 2022. Watch sessions on your own schedule and earn up to 50 CME credits/MOC points.
Don’t forget to claim your credit! The deadline is December 15, 2022, at 11:59 pm CT.





